Celebrities are just people like us and we put it that way, it’s shocking, right? The beloved, Julia Louis-Dreyfus, Veep star, and Seinfeld alumna, seemingly ageless sitcom staple since the 1980s, has recently revealed she has breast cancer.
She tweeted: “The good news is I have the most caring and supportive group of family and friends, and amazing insurance through my union. The bad news is not all women are as lucky as me, so let’s together fight all cancers and make universal health care a reality.”
Inspired by that fight, we reached out to nutritionists, doctors, and other health experts and asked them for their best pieces of advice for fighting breast cancer. Stay with us to stay healthy for life. The following are expert advice about prevention, diagnosis, and treatment of breast cancer, you must know!
PREVENTION
1Quit Smoking and Limit Your Alcohol Intake
As a woman, you’ve already got the chances to face breast cancer, however, lifestyle plays a significant role, as well. “We do have significant information regarding other risk factors, thus, there are things that women can do to reduce their risk of breast cancer. We have studies demonstrating that excessive alcohol intake and smoking increase the risk,” says Dr. Robert Coke, an intensive care and internal medicine practitioner at McMaster University. Also, there are many other amazing benefits if you limit your alcohol and quit smoking, besides lowering the risk of breast cancer.
2Keep Your Weight in a Healthy Range
Dr. Coke claims the women with extra kilograms are at an increased breast cancer risk as well. So, she recommends maintaining a healthy weight since it can seriously reduce the risk of developing breast cancer.
3Limit Hormone Therapy
Dr. Anne McTiernan of the Fred Hutchinson Cancer Research Center says progesterone-based menopausal hormone therapy may increase your cancer risk. She suggests avoiding those that contain progesterone if you must take hormones to manage menopausal symptoms. Also, she advises limiting their use to three years. It goes without saying that you should always consult your doctor before stopping or starting any medication.
4Get Screened Regularly
All women, especially those with a family history of breast cancer, regular mammograms on a doctor-prescribed schedule are very important. Also, dr. Coke says that getting regular screenings is your best option for detection. She says those women could reduce their risk of developing the metastatic disease by being screened regularly. So, keep in mind that there are many lifestyle changes you can make to reduce your risk, however, getting regular screenings is necessary.
5Know Your Potential Risk Factors
Dr. Shafer. says there are also hormonal risks like early menstrual periods and late menopause that could be a predictive factor, besides a family history of breast cancer. But if you have a family history of breast cancer, then it’s essential to have tested and discussed the results. Dr. Shafer says after the results together with the doctor you will determine if monitoring or proactive preventive surgery is the best option.
IF YOU SUSPECT SOMETHING IS WRONG
6Get Checked Any Time There’s a Change
Any change in your breast tissue requires a visit to the doctor. Women, especially the pregnant and breastfeeding women mistake potentially-cancerous lumps for hormonal changes. Sullivan says a few clients thought they only had a clogged duct but left with a breast cancer diagnosis upon the visit to the doctor.
7Don’t let the Biopsy Scare You
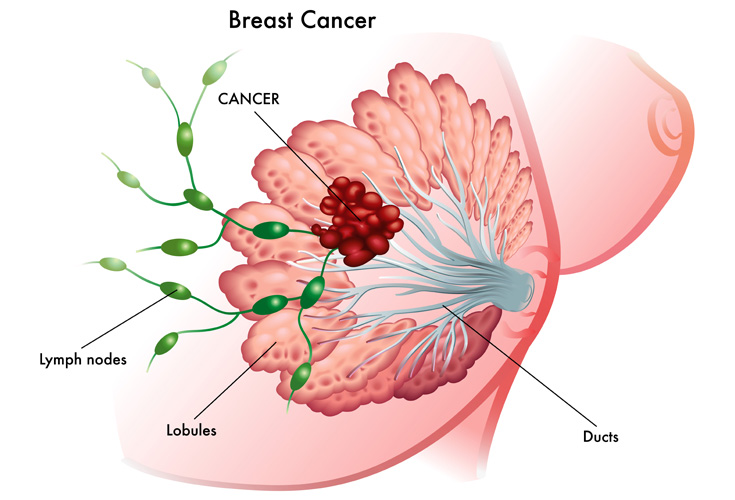
Dr. Lyda E. Rojas Carroll, MD, FACS, a breast surgeon at Caremount Medical explains a biopsy can be done using either a Magnetic Resonance Imaging (MRI) or an ultrasound mammogram. “This radiographic testing along with a breast exam can tell you the size of the tumor and if lymph nodes look or feel abnormal,” she adds. The biopsy will reveal the type of cancer and whether the cells are sensitive to HER-2/neu and estrogen-progesterone. Dr. Rojas Carroll says if the breast is dense or an invasive lobular cancer had been diagnosed, an MRI of the breast might help plan the surgery.
UPON DIAGNOSIS
8Get a Personally-Tailored Diet Plan
Going through radiation or chemotherapy can change the taste buds and create gastrointestinal issues. So, Lewis-Huebel suggests consulting with a Registered Dietitian (RD) to manage nutrition needs that are unique for patients.
9Maintain Your Activity Level
Dr. Fremonta Meyer, a clinical psychiatrist from the Dana-Farber Department of Psychosocial Oncology and Palliative Care, says that regular exercise can help with the memory-depleting effects of chemotherapy. “Chemo brain” is a term used to describe memory problems and foggy thinking that can happen after the treatment. So, keep exercising or at least walking as much as possible.
10Cut Out Supplements
Dietitian Suzanne Gerdes, MS, RDN, CDN of Memorial Sloan Kettering Cancer Center says they want their patients to avoid supplements that are not prescribed from them. The reason for that is the patients take so many medications, so they are not sure what’s going to interact with the supplements.
11Even Invasive Cancer Can Be Cured
Dr. Amber Guth, a breast surgeon and associate professor of surgery at NYU’s Langone Medical Center says 75% of cancers diagnosed in the United States are considered early stage, either stage 0, I, or II are generally considered curable. He adds there are many promising treatments available today even for phase III, despite it doesn’t have a high cure rate.
12Don’t Be Scared of Your Changing Body
Reconstructive surgery has come a long way. “The way they’ve been able to restore tissue is amazing,” says Sullivan. Now, the doctors can make incredible things with tonal matching for skin grafts. Also, tattoos can help create a natural look for areolas.
REGARDING RECONSTRUCTION
13Implants Can Look Natural
Dr. Kolker says there has been a major advance in the types of implants they use. Now the implants are teardrop shaped and look more natural. He also points to the improvement of techniques like fat grafting in making a more natural look after the surgery.
14Plastic Surgeons are not Only Concerned With Aesthetics
Dr. Kolker says that their task, as plastic surgeons, is to restore that sense of self, that sense of balance. For them is much more than simply replacing that tissue that’s been removed. They are hoping that you will feel better in your own body and get back your confidence!
15You may use Your own Tissue for Reconstruction
Let’s be clear, the likelihood of being able to use your own tissue instead of an implant must do with your body type. Dr. Kolker says some women may have no extra tissue to work with. Also, dr. Kolker says for most women who have reconstructive surgery, implants aren’t the first and final step. They put in a tissue expander first, then an implant. This is a part of a 2-stage implant reconstruction.




